Many people are curious whether or not that fever, ache, or cough means they’ve had the coronavirus. Unfortunately, due to a widespread lack of testing, most suspicions remain just suspicions without an official diagnosis.
New antibody tests, which are available in physicians' offices, urgent care centers, and laboratories, may provide some answers. There are more than 70 COVID-19 antibody tests on the market because of the urgent situation, but only four are approved under the FDA’s emergency use authorization (EUA) process. Still, many companies are allowed to use their tests on patients to gather more data, especially to determine just how widespread the novel coronavirus could be throughout our population. A random sampling of 3,000 people in New York discovered that potentially up to 25 percent of New York City residents have been infected with the coronavirus already.
The test I took, which was manufactured by Quest Diagnostics, was not FDA approved — but could provide clarity for me and others around me.
COVID-19 tests look for antibodies, which are proteins the body develops in response to toxic or foreign substances inside the bloodstream. They help the immune system get rid of outside pathogens. The specific test I took was looking for COVID-19 Immunoglobulin G (IgG) antibodies, which are what researchers look for to determine if a person has immunity against a disease after taking a vaccine. Another kind of antibody, Immunoglobulin M (IgM), is the first antibody produced when you have an infection, although it doesn’t necessarily mean you have immunity. This kind of antibody has been found in some people who were recently infected by the coronavirus or had a mild case of the disease.
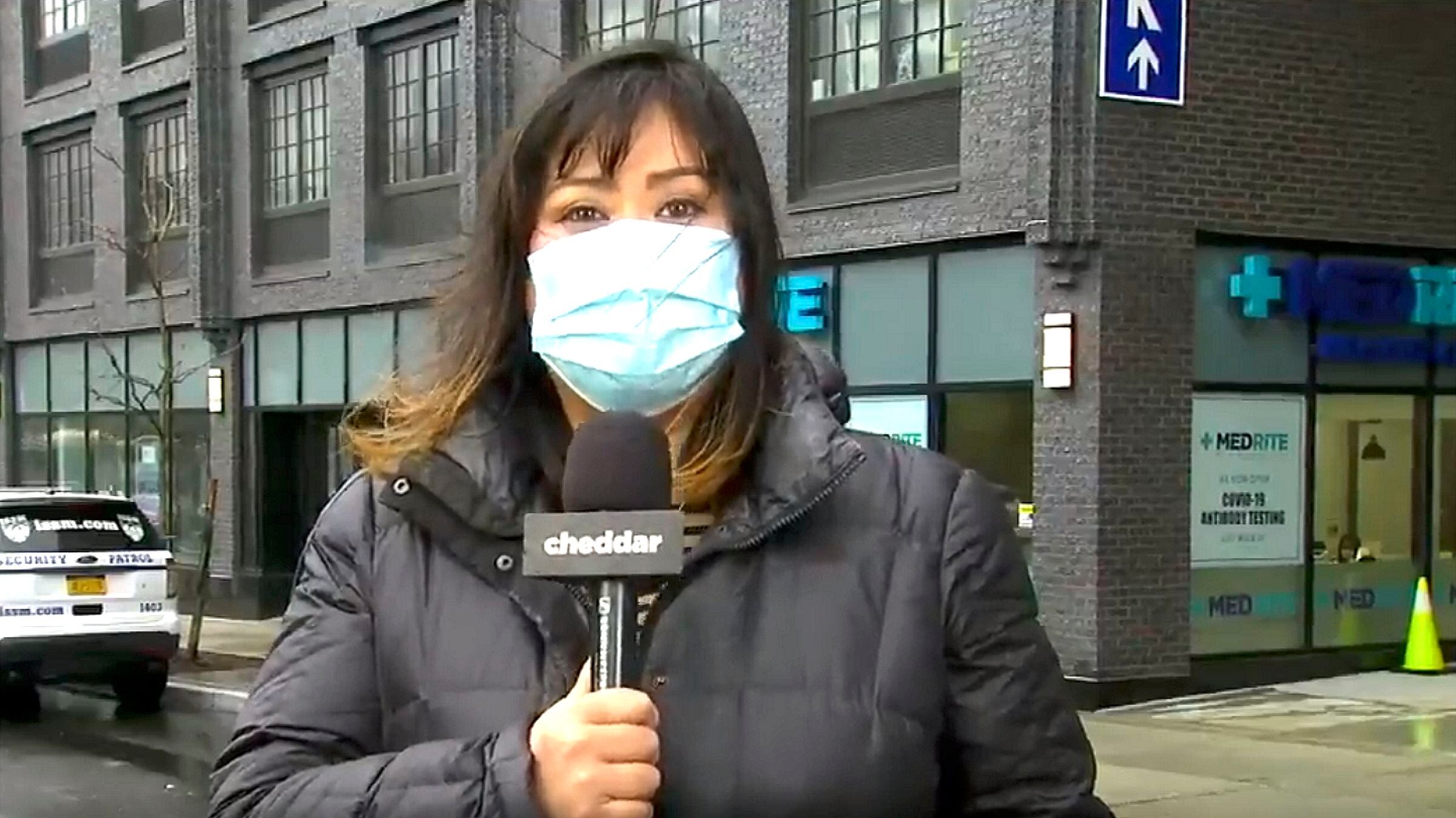
When I approached MedRite Urgent Care in the Clinton Hill section of Brooklyn, New York, there was a sign to the right of the building asking people seeking COVID-19 antibody testing to line up. There was no one in line, but as soon as I arrived in the designated area a security guard with a face mask on came out and asked me if I was seeking testing. He then asked if I felt ill. I responded that I was looking for the antibodies test and did not have any coronavirus symptoms.
He then escorted me inside and asked me to sit down. I was already wearing a mask but had I not been, I would have been required to put one on to enter the facility. He handed me a clipboard and a pen and had me fill out some basic paperwork with my information and a short questionnaire to indicate whether I felt sick. When I was done, I waved him over and he took my forms, my ID, and my insurance card to the front desk. I could hear them spraying down the clipboards with disinfectant between use. The cost of the test was $50 plus a $125 visit fee, but most insurances cover part, if not all, of the visit and test.
There was someone who entered the urgent care with a more pressing matter, so I had to wait. However, my name was called within 20 minutes and I was escorted into an exam room.
The medical professional told me the COVID-19 antibodies test was a simple blood draw and asked if I had any questions. She asked me if I was feeling ill and then proceed to take my oxygen levels with a pulse oximeter. She also took my temperature, which was a healthy 98.5 degrees Fahrenheit. She again reiterated my test would not tell me if I have coronavirus, but only if I potentially had it previously.
After my blood draw, a physician’s assistant came to my exam room to answer any additional questions. She said the test was qualitative, not quantitative, so it would only tell me if I had COVID-19 IgG antibodies or not. She also admitted scientists still don’t know if COVID-19 antibodies offer immunity and for how long, though typically with other coronaviruses, immunity occurs for some period after a person is infected.
In an ideal world, she would be able to provide me with a PCR test, otherwise known as the nasal swab test, in addition to an antibody test to determine if indeed I had contracted the coronavirus. Most blood banks require both the PCR test and the antibody test to donate plasma. She said it might be worth checking with my local blood banks to see if they’ve eased restrictions to allow people with antibody tests to help out.
More than 200 people per day come to her MedRite site to get tested, she explained. Some were presumed positive by doctors but weren’t able to get tested. Others are just curious, even though they have been indoors for more than two weeks and don’t even go out to get groceries. Antibody tests may also become a requirement for employers to allow people back to work. However, a positive test does not necessarily mean I'm immune or can’t spread the disease to other people, so she emphasized I should continue to wash my hands and wear my mask outside. She ended by telling me I would get the results in two to three business days. I said goodbye, walked out of the urgent care center, squirted some hand sanitizer on my hands, and pulled up my mask a little higher.